'Working with Diverse Audiences' - Talk & Presentation May 2011
Fabrica May 2011- Rendezvous Programme - FABRICA
This is a synopsis of a 90 minute presentation with some additional thoughts.
• talk was given to an intimate peer group audience made of of artists and health professionals
- As audience settled a video entitled 'The Passion' by Rosemary was on screen
Note - All audio-visual material has been granted permission by the contributors for public viewing.
I was happy to be invited by Fabrica to give this talk as I felt that it was time to reflect on my work in healthcare both as a practitioner creating art & design for health environments and also as part of a large psycho-social team, as artist-in-residence in Trinity Hospice, London. This team delivered a varied care package to individuals & families both in hospice and as outreach. I am now seeking ways to 'converge' this broad experience working within relevant positions or pro-actively initiating further projects

Background
My 25 year career in the arts began with a 10 year period working as a Performance artist creating live installations where the audience had an important interactive role in shaping the direction of choreography, space and environment. This performance and subsequent physical theatre work generally required and thrived from audience participation and manipulation, sometimes to the point whereby my safety as a performer was compromised. It was definitely a time of testing my emotional and physical thresholds, whilst at the same time exploring established boundaries between audience and performer. In certain street performances I was bottled, physically threatened and assaulted. In more controlled environments I was fortunate to have some memorable experiences and audience contact which I continue to this day to process and contemplate both as protagonist but also with those that shared it.
My interest in healthcare lies within the opportunity to effect positive change in the built environment. My early work in performance, I believe, shapes how I view public buildings, their daily cycles, and the myriad of roles played out within by the staff and users. As an artist working on these environments, one has to be aware of what is expected of you, and act accordingly. In projects where lead artist roles are required to develop an art and design strategy within new build or large refurbishment projects, this role is pre-defined, and the artist takes on more of a consultancy role and is usually a member of a core design team. In later years I ventured into 'Public, digital and interactive art' and now have made a body of art & design work which has been made calling upon skills & experience gained in various methods of art production.
Artist's sometimes can't help themselves but challenge entrenched forms of institutional behaviour and can act as an important bridge between stakeholders, staff and third party interests in the design process. In institutions which are in a sensitive transition process, for example a move from old buildings to new...they can act as creative brokers between 'the public' and the organisation, yet still retain authenticity within an individual approach. People in the Uk still feel a strong sense of ownership of the NHS and it is this passion that should be harnessed to design and build environments which are models of best practise for all stakeholders.

We also have to be mindful that sometimes all hospitals want and need is some good art & design…and why should we argue with that? There is a growing body of evidence that supports the need for good basic art & design in healthcare environments. There isn't one research body that collates all this research but a good place to start looking is the Arts Council's literature review which is dated 2004.
http://www.artscouncil.org.uk/publication_archive/arts-in-health-a-review-of-the-medical-literature/.
When you begin to dig, you can find much research to back-up most forms of creative activity within hospitals and healthcare. However, it is very dry research and there remains a large vacuum for a researcher to compile a publication on this interesting area....perhaps it is being written as I am writing this. It wouldn't hurt to do some serious scientific research into the effects of lighting, wall colour, good design & way-finding etc.
I believe that simple changes can bring huge benefits. For example...I have been in situations where I have proposed the specifying of one or two brighter colours for a 400 metre long corridor rather than an off-white or magnolia, these are the spaces that affect peoples lives moods and focus for 365 days a year, day-in day-out. This might sound simple...it is not, and can be an uphill struggle to even effect minor changes within a large institution.
Most of the work in larger projects is hidden and forms the prosaic tasks of designing, managing, producing, advocating and installing artwork which has been rubber stamped by committees, fund-raisers and users. The culture of art & design production is changing thankfully to from an 'us & them' approach to artists being part of a core design team. This saves time, money and presents opportunities where art can be built into the fabric of the building rather than an after thought.
There are many scenarios where this experience can be utilised. In large hospital new
-builds, for example, consultation with users and staff is part of the lexicon of design & build. Stakeholder representation and input is now embedded in hospital culture. However, this also creates another new layer of management…more meetings, more demands on staff schedules, so it must be done with sensitivity to existing managerial frameworks.
Few architects, designers or artists have intimate knowledge of the raised anxiety levels, emotional stress or physical ailments that are presented every day to health practitioners and carers. However it is safe to assume that all of us will at some stage of our lives, whether that is to give birth, be treated for an injury in A & E, or visit a relative or family member being treated for an illness, use the services of our health service.
This is why the healthcare environment is of interest to me. It serves everyone, it is incredibly diverse in the care delivered and the physical spaces which deliver the care, and the Uk is going through a seismic psychological shift from smaller care centres to huge regional hospitals that provide a whole range of care under one roof. The Uk is also suffers from a plethora of older buildings ranging from pre-florence nightingale to the present day. It is an area of design, architecture & design which can have a direct and tangible subliminal or psychological impact on the building user, hopefully in a positive way.
BHOC (Bristol Haematology & Oncology Centre) - a recent healthcare Project

- a short evaluation of my most recent project where I acted as 'Lead Artist' on an art & design refurbishment for the BHOC.
Various art & design solutions where employed to maximise the potential of an existing budget of approximately £50,000 to provide uplifting environments for reception areas, waiting rooms and art installations that provided orienteering mechanisms within the building. A way-finding strategy was also developed that used large vinyl graphics as floor level markers for life exits and stairwells.
Broad range of approaches were used within existing and immovable design specifications, including photographic original prints & narratives derived from authentic artistis research in the cal environment, thus embedding the imagery within a local framework. Bespoke artworks (MUG installation, Quilt artwork & Lift Light-box works), Large vinyl wall graphics & bespoke laminate tables. It also included large portions of stakeholder consultation and contributions to various artworks. This project has been short-listed for a Building Better Healthcare (BHH) award (Best use of Visual arts in healthcare) to be announced in November 2011. http://www.bbhealthcare.co.uk/show.php?

Palliative Care Work
I come from family who have almost 100% (on one side) been involved in medical care or health provision in many forms so it seems natural for me to be involved in this field of work.
I was originally appointed as a 'digital artist in residence' at Trinity by Rosettalife, an organisation who has an impressive track record of initiating creative placements and projects within palliative care environments. Now, a few years on, many artists who had posts within hospices have suffered from the economic pressures of the times and have had there contracts terminated. But let's move on from talking about the economic times we live in...this work immediately presents us with difficult scenaros.
How do you enagage someone in a meaningful way, culturally and emotionally amidst the baggage and clinical reality of dying.
PAIN / FEAR / ANXIETY / MEDICATION / FAMILY LOVED ONES / CARE STRATEGIES / FUTURE PLANS WILLS / GETTING THROUGH TODAY
"I feel like an investigative journalist, searching for kernels of truth and armed with only a camera, trying to get decent footage with little time amongst the whirlwind of clinical terminal care..."
Chris Rawlence - Director of Media Rosettalife.
There are many contradictions that surface whilst working as an artist within institutions. On the one hand, I saw for myself how energising and positive creative intervention at the final stages of life can be. On the other hand, from a clinical perspective, why should it be the responsibility of a hospice/healthcare institution to deliver forms of creative contact, explore the meaning of life, or exploring one's identity (for example)? In 2008 the government published the 'End of Life Strategy'. A report that states that amongst many objectives, we need to provide services that are more person centred, that cater for the needs of a highly complex society. Art & creative intervention can act as a bridging mechanism between user and management in palliative care and other healthcare scenarios. It allows us to all think of ourselves as 'significant individuals' within a system where we are all stakeholders.
A social worker who shall remain nameless for issues of confidentiality once said of Trinity Hospice (although I'm sure he wouldn't mind being named) -
" What this place needs is more Sex, drugs & Rock & Roll"This translates as - If we are to care diligently for a age of people with lifestyles then who are we to say what they get up to in their private rooms? We did actually get a visit from Lemmy from Motorhead as he was visiting an old friend. I would have got his autograph if only I'd have been on duty…(provokes thought of new Kronenburg advert..yes we all have to slow down sometime.) http://youtu.be/khJKq_kJK7Q
Some people I have been privileged to have worked with.
Note on Equality of care.
How does one give equal care to a broad range of backgrounds, narratives and wide range of extreme physical decline? Contact time ranged from years to 5 minutes. How do you train to be able to engage in a meaningful way with a 32 year old crack addict mother of two on high dosages of pain relief (& therefore 'medicated'), who is about to die? Surely the time spent attempting engagement is as important if not more, than the creative products of work with people who understand the lexicon of creative expression. The majority of people I worked with had not done anything creative (in their opinion) since they had been at school.
You do what you can, you listen, act and attempt to make contact or dialogue. You try to make something even a small audio recording. You try to make something more substantial if there is a will and a way. Sometimes witnessing is enough and incredibly important.
I played a short audio recording of an 83 year old woman who had needed someone to witness her story of being sent by her mother to England, aged 12 from Vienna. Her mother and some of her immediate family subsequently died in Nazi concentration camps. Her reason for wanting to document this was because everyday of her life she had felt incredible guilt about not being able to save her mother and aunt. In her words, she had lived a 'nightmare' everyday of her life because of her guilt. I believe that she had not been able to discuss this with anyone during her lifetime and the recording was passed on to her family at her request.
DAVID
David is one of the first people I worked with and because of this had a relationship lasting three years. He was someone who used his predicament to lobby those in positions of influence to effect positive change both in the hospice movement and within his local borough of Lambeth. He gained notoriety for this approach and our work became part of this process. He had burmese carers so naturally was interested in the Burmese uprising in 2007 so we agreed to make a short film of shaving his hair off in solidarity with the Burmese monks. This became also a potent metaphor for his own story, purification or preparation for death. Most days he wore a shirt emblazoned with "I'm not dead yet". This was a visual response to everyone that asked him "How are you today?", using ironic humour to mock our inability to discuss debilitating illness in a straightforward way. I asked him how he would prefer to be greeted...I suggested " How don't you do?" as a possible replacement.
We filmed with the help of a PHD student Naomi Richards in an ad-hoc studio set-up in his sheltered accommodation communal hall, taking a series of stills throughout the process. I chatted to him atempting the role of a mockney barber and asking him about the troubles in Burma. The result was a time-based auto portrait that simply plotted his evolution from hirsuit to shaven headed. It has no audio and allows us the audience to see david in a state of metamorphosis, the context of his illness hints of changes to come and the transition that we all must make from our physical state.


"my father once said to me...the brain is like a freshly-mown lawn, whereby if you tread in it the grass will spring back to the shape it was.."
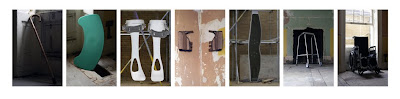
Theresa used her work with me as a bridge to talk about how she felt day to day within her own personalised care strategy. She suffered from the degenerative disease of Motor Neuron Disease (MND), a disease with a usual prognosis of death within 4 years from detection. She had long relationship with the hospice and her eventual death affected everyone that had worked with her over her time as an out-patient and inpatient. I assisted her in making portraits of herself, no, correction…portraits of the objects that she has used or assisted her during her physical decline. She then used this image, with my assistance as a way of discussing between departments, how she felt that she was 'seen' by staff within the hospice. We like to say things like, 'You are so brave Theresa' but all she wanted to express was the fact that most days she felt crap and weak, and not at all …brave. This inter-departmental meeting hosted by myself with theresa surprised everyone by allowing an outpouring of emotion from everyone in the room, a moment of release that was refreshing in an environment where it is difficult to speak the truth for fear of upsetting anyone.

'Nippy' - Terri © 2010
Anna
Anna was gravely ill and did not suffer fools gladly. She had written poetry ever since she was young. I don't not know how many people have read her poetry in her lifetime. She needed, but didn't ask for, help to type, edit, design a simple layout for a book and publish it online...where it now resides to be bought by anyone. It exists as a testament to her mysterious life and work.
I read one of her poems to finish this presentation, and realised that as I spoke, it might have been the first time anyone else has heard her written words...almost a premonition. She wrote the poem aged 25.
Poem written Bedford Styvensen Brooklyn N.Y.C 1981
for Eileen Orwell & me
These tragic women
whose tragedy is my own
and not my own
Who die in northern England
nursing homes
of cancer
when dusk is falling
Who fade on remote country estates
of terror shock and sheer heartbreak
when their one child is murdered
by the rougher males
in Brixton or Eton
these women of the haunted eyes
and secret sorrows
and buried lies
lost in unshed tears
as grey as England
as cruel and un cried
as those whose gaze i cannot bear
whose dreadful power loss I share
even as I thank the God
I was born far away in warmer shores
bearing blood of a different race
whose hatreds I will also
not escape
I pray that when I die
I may learn to die not like them
spare me the deaths of English women
in the secret cells
of grieving at the cruelty
and coldness
pitched beyond believing
Let me not fade away
in that dreadful unclaimed sorrow
where land dissolves beneath your feet
in hideous slow motion
onto the crumbling suns and sins
and sons of England
in dishonest ancient Britain
Down and out
in Paris, History, or London
Synopsis
Many institutions do not have an open culture of debate, where positive contributions can be discussed and a natural dialogue between staff and management creates an exciting culture and creates it's own momentum. This is unfortunate for those who wish to modernise or improve the overall quality of holistic care.
Most complimentary services in healthcare are entrenched in inter-departmental tension, each vying to be taken seriously, each competing for funds (more so since the 2008 recession) alongside important clinical provision. In my opinion a progressive organisation should have an open culture of debate, allowing new ideas to flow naturally and help in the modernisation of societies' attitude towards death & dying, an ageing population and ultimately the provision of better care, in keeping with the goals of the End of Life Strategy.
I do not see creative intervention as 'complimentary' - nor do I consider therapeutic massage, counselling, bereavement work and other forms as 'complimentary'.
This devalues it substantially and the origin of the language perhaps hails from 80's corporate culture…as if it is a complimentary biscuit on the side of the saucer of the all important clinically proven tea & coffee. I speak as an ITEC trained masseur so I know the numerous benefits massage can have.